This website requires you to be 21 years or older to enter. Please confirm your age below to continue.

Fibromyalgia (FM or Fibro) is a debilitating chronic disorder affecting an estimated 10 million people in the U.S. and an estimated 3-6% of the world population. Living with the condition can be incredibly painful. The most common symptoms include – widespread musculoskeletal pain, extreme levels of fatigue, problems with cognition, and very poor sleep quality. And, unfortunately, there is no cure.
What’s the cause?
Fibromyalgia literally means “muscle and fibrous tissue pain.” The pain can occur all over the body but is usually felt near the joints. Fibromyalgia belongs to the category of rheumatic diseases and is a complex condition that is not widely understood. However, researchers believe the pain may be caused by hypersensitivity to stimuli that, under normal circumstances, would not be painful. In other words, the condition occurs when the body doesn’t process pain normally.
There is a range of likely risk factors, including:
Fibromyalgia may also be hereditary. In addition, traumas such as abuse in childhood, current psychological stress (relationship conflicts, financial strain, health problems) can promote the development of the disease.
As mentioned above, there are also some illnesses and infections that can either trigger the condition or aggravate it. Certain types of emotional or physical trauma can contribute to fibromyalgia, and it has also been linked to post-traumatic stress disorder (PTSD).
While it is more common in women (75-90 %), it also affects men and children of all ethnic groups. The condition is frequently found in families, such as between siblings or between mothers and their children. The diagnosis is usually made between the ages of 20 to 50 years, but the incidence rises with age so that by age 80, approximately 8% of adults meet the American College of Rheumatology classification of fibromyalgia.
A brief look into the history of Fibromyalgia
Fibromyalgia is a disease that’s been affecting individuals for centuries. Our understanding of the disease has transformed over time and is still evolving.
As evident through its history, fibromyalgia, and treatments for this disorder have been evolving since first discovered. While science and medicine continue to improve drastically, in many ways, fibromyalgia still remains a mystery.
Here are some important advancements
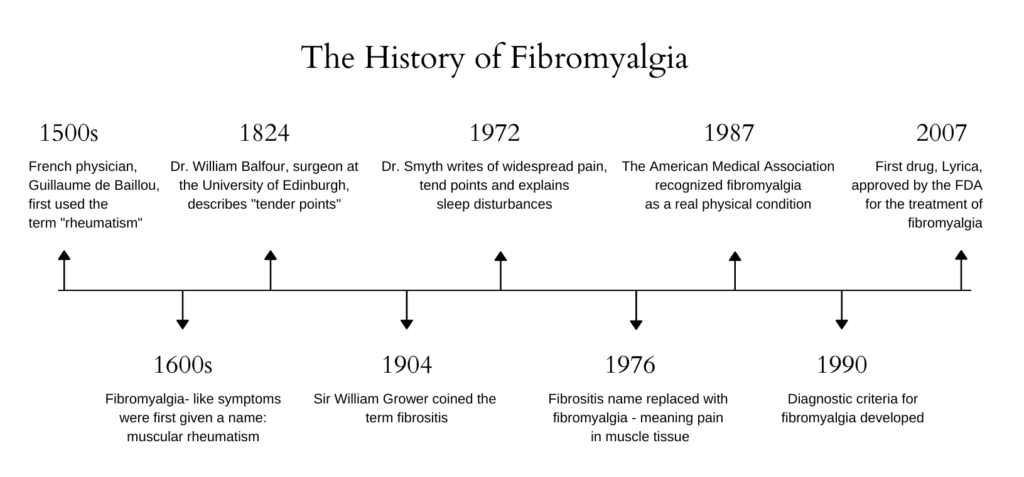
In 2010 the American College of Rheumatology released alternate diagnostic criteria using questionnaires instead of tender points. And in 2014, researchers confirmed that underlying endocannabinoid deficiency indeed plays a role in fibromyalgia.
Researchers are looking into possible new factors including, inflammation of the facia, extra nerves on blood vessels, small-fiber neuropathy, and immune system abnormalities. Several researchers also are working to establish subgroups of fibromyalgia, believing that it’s the key to nailing down the underlying mechanisms and best treatments.
Fibromyalgia and Clinical Endocannabinoid Deficiency (CED)
The endocannabinoid system (ECS) is a cell signaling system (think of it as a traffic controller) in your body regulating numerous bodily functions helping you remain balanced. Today, research has linked the ECS to a variety of bodily functions and emotions.
The ECS is made up of endocannabinoids – molecules that send messages; and cannabinoid receptors CB1 & CB2 – the receiver of the messages. One of these types of receptors, the CB1 receptors, are found in your central nervous system. The central nervous system is responsible for regulating pain.
Clinical Endocannabinoid Deficiency (CED) is a theory that proposes – lower endocannabinoid levels in one’s body can lead to conditions like IBS, fibromyalgia, and other treatment-resistant disorders.
In 1998 research showed that endocannabinoids could reduce increased sensitivity to pain (hyperalgesia). This finding has led researchers to believe that cannabis, or specific cannabinoids in cannabis, can help treat certain symptoms of fibromyalgia. What has been proven time and again is that cannabinoid therapy can help the endocannabinoid system operate more smoothly.
Fibromyalgia signs and symptoms (just a few)
Other symptoms may include:
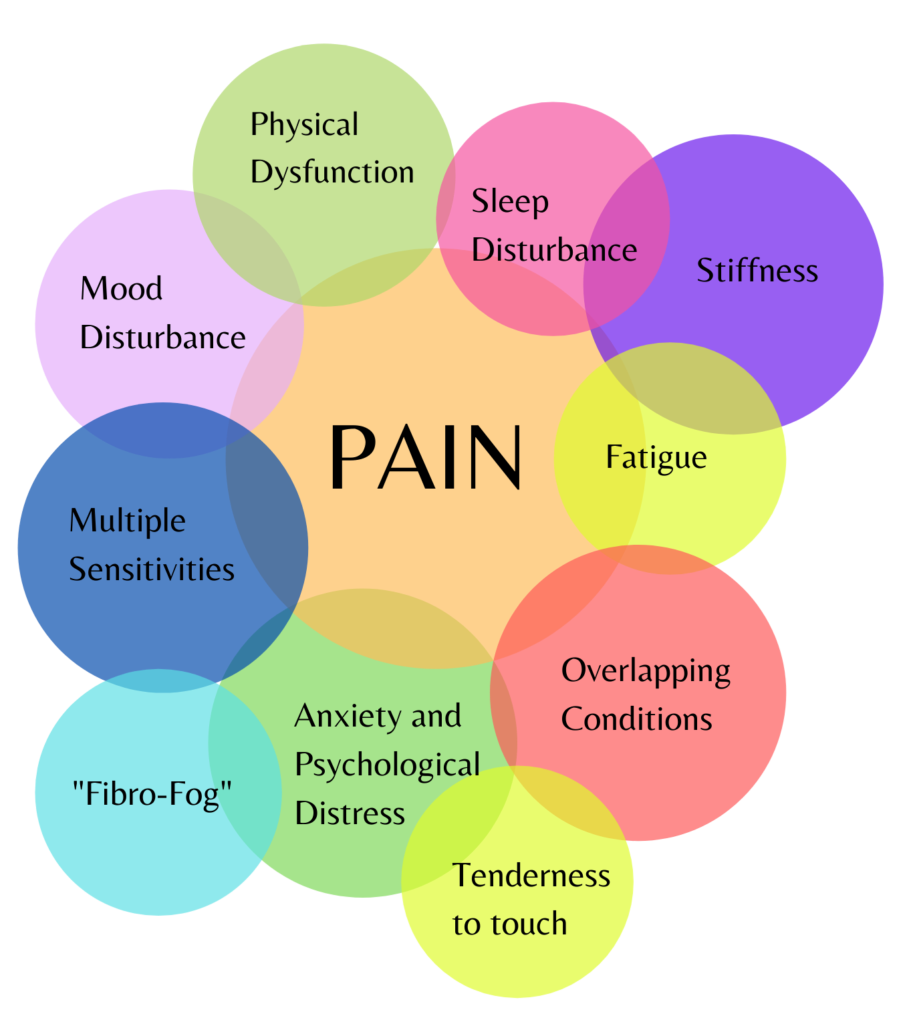
Often, overlapping conditions such as temporomandibular joint disorder (TMJD), irritable bowel syndrome (IBS), headaches and migraines, anxiety and depression, and environmental sensitivities co-exist with fibromyalgia.
Medical treatment
Current medical treatments are often limited to a combination of pain relief medication, antidepressants, muscle relaxers, and sleep aids. Sometimes physiotherapy or other lifestyle changes, such as low-impact exercise, like Tai Chi, are also recommended. But these treatments don’t work for everyone, and sometimes the medication prescribed can come with a multitude of unfortunate side effects.
Because of these limitations, many fibromyalgia patients have continued to experiment with different methods of managing their pain, such as cannabis.
Can cannabis help treat Fibromyalgia?
The answer in many cases is yes. Many patients with fibromyalgia report several benefits from cannabis use but, until recently, we did not have the studies to back it up. In 2019 a study using both THC and CBD reported being very beneficial in the treatment of fibromyalgia. The study demonstrated how cannabis has pain-blocking effects on chronic pain patients with fibromyalgia.
Many studies related to cannabis treatment for muscle spasms assume the spasms are caused by inflammation.
Since fibromyalgia doesn’t involve inflammation, not every study is relevant. Studies that focus on muscle spasm causes besides inflammation have promise.
The symptoms of fibromyalgia are theorized to be caused by your brain misreading pain signals, so cannabis could be a vital treatment.
Recent studies show that cannabinoids might be a useful treatment option for patients with fibromyalgia. For example, researchers from the Clinical Cannabis Research Institute in Israel have analyzed data from fibromyalgia patients between 2015 and 2017 in a prospective observational study. The result: 81% of the study participants noticed a positive effect from cannabinoid therapy.
Cannabis is known for treating anxiety, depression, fatigue, sleep disturbances, and more.
In fact, one of the prime benefits of cannabis is its versatility. Most strains treat multiple symptoms, but you can find strains that treat a specific set of symptoms as well. Since fibromyalgia is a multifaceted illness, cannabis may help more than one symptom and reduce the number of medications you need. Less medication equals fewer side effects and damage to your liver.
Final thought
While further research is necessary, the future for treating fibromyalgia with cannabis looks promising and could confirm what many patients have already experienced – relief.
Would you like to learn more about how medical cannabis can help treat fibromyalgia? Plant Family Therapeutics has a medical cannabis consultant who can help find the right cannabis medication and dosing for your needs safely.
References
Fiz, J., Duran, M., Capella, D., Cabonell, J., & Farre, M. (2011). Cannabis use in patients with fibromyalgia: Effect on symptoms relief and health-related quality of life. PLoS One. 6(4),e18440. doi: 10.1371/journal.pone.0018440
Giamberardino, M. A., Affaitati, G., Martelletti, P., Tana, C., Negro, A., Lapenna, D., Curto, M., Schiavone, C., Stellin, L., Cipollone, F., & Costantini, R. (2015). Impact of migraine on fibromyalgia symptoms. The journal of headache and pain, 17, 28. https://doi.org/10.1186/s10194-016-0619-8
Giorgi, V., Bongiovanni, S., Atzeni, F., Marotto, D., Salaffi, F., & Sarzi-Puttini, P. (2020). Adding medical cannabis to standard analgesic treatment for fibromyalgia: a prospective observational study. Clinical and experimental rheumatology, 38 Suppl 123(1), 53–59. https://pubmed.ncbi.nlm.nih.gov/32116208/
Habib G, Artul S. Medical Cannabis for the Treatment of Fibromyalgia. J Clin Rheumatol. 2018 Aug;24(5):255-258. doi: 10.1097/RHU.0000000000000702. PMID: 29461346
Lochte, B., Beletsky, A., Samuel, N., & Grant, I. (2017). The use of cannabis for headache disorders. Cannabis and Cannabinoid Research 2(1). https://doi.org/10.1089/can.2016.0033
Richardson, J. D., Aanonsen, L., & Hargreaves, K. M. (1998). Hypoactivity of the spinal cannabinoid system results in NMDA-dependent hyperalgesia. The Journal of neuroscience : the official journal of the Society for Neuroscience, 18(1), 451–457. https://doi.org/10.1523/JNEUROSCI.18-01-00451.1998
Russo E. B. (2008). Clinical endocannabinoid deficiency (CECD): can this concept explain therapeutic benefits of cannabis in migraine, fibromyalgia, irritable bowel syndrome and other treatment-resistant conditions?. Neuro endocrinology letters, 29(2), 192–200. https://pubmed.ncbi.nlm.nih.gov/18404144/
Russo EB. (2008) Cannabinoids in the management of difficult to treat pain. Ther Clin Risk Manag. 4(1):245-59. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2503660/#!po=53.4483
Sagy, I., Schleider, L., Abu-Shakra, Mahmoud., & Novack, V. (2019) Safety and efficacy of medical cannabis in fibromyalgia. J. Clin. Med. 8(6),807. https://doi.org/10.3390/jcm8060807
Smith, S. C., & Wagner, M. S. (2014). Clinical endocannabinoid deficiency (CECD) revisited: can this concept explain the therapeutic benefits of cannabis in migraine, fibromyalgia, irritable bowel syndrome and other treatment-resistant conditions?. Neuro endocrinology letters, 35(3), 198–201. https://pubmed.ncbi.nlm.nih.gov/24977967/
van de Donk, T., Niesters, M., Kowal, M. A., Olofsen, E., Dahan, A., & van Velzen, M. (2019). An experimental randomized study on the analgesic effects of pharmaceutical-grade cannabis in chronic pain patients with fibromyalgia. Pain, 160(4), 860–869. doi: 10.1097/j.pain.0000000000001464
Walitt, B., Klose, P., Fitzcharles, MA., Phillips, T., & Häuser, W.(2016). Cannabinoids for fibromyalgia. Cochrane Database Syst Rev.7(7) CD011694.https://doi.org/10.1002/14651858.CD011694.pub2