This website requires you to be 21 years or older to enter. Please confirm your age below to continue.
For the last decade, the conventional approach to understanding and treating depression was to think of it as a chemical imbalance. That is, there are insufficient amounts of the neurotransmitters serotonin, norepinephrine, and dopamine in your brain, and the low levels of these brain chemicals are what is causing your depression. Depression is then treated by replenishing these chemicals with medications that help the brain cells or neurons either produce more of the chemicals or stop the chemicals from being broken down after they are produced so that they hang around a little longer. This is the concept behind the SSRIs or serotonin reuptake inhibitors.
Researchers now know, through studies using functional MRIs, genetic biomarkers, post-mortem dissection of the brain, and monitoring the brains of mice, the reason neurotransmitters are low is due to disrupted neural circuits in the brain. It is related to the concept of neuroplasticity. With depression, you get negative neuroplasticity.
Neuroplasticity is the process of the brain remodeling itself over time as we learn new things. Think of your brain as your computer’s central processing unit that functions through a complex circuit. The circuit is made up of neurons which are nerve cells. As you learn new things, new circuit paths are formed, and old unused paths disappear. These paths are just simply the nerve cells connecting to one another. The cells communicate by secreting chemicals. These neurotransmitters become the ways that the cells transmit information.
Donald Hebb was a psychologist who developed the theory called; Hebbian theory of how nerve cells function in the brain. The catchphrase of his theory is that – neurons that fire together wire together, and neurons that fire out of sync failed to link.
How does this relate to depression?
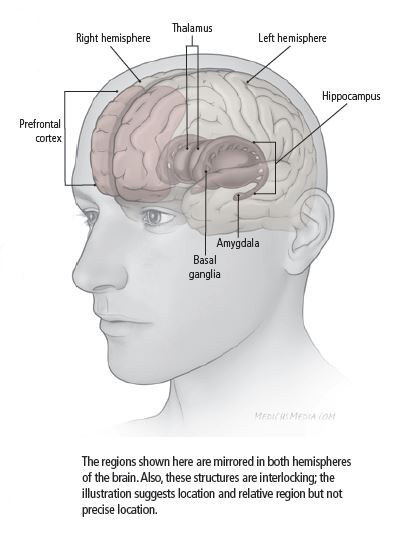
With depression, there is a disconnect between certain neural circuits, and these circuits are mostly in the prefrontal cortex and our hippocampus. These are the areas of the brain that regulate mood and information processing. So instead of the neurons firing together, the circuit link is broken, and this is where you get inadequate amounts of serotonin, norepinephrine, and dopamine.
So, researchers know what is happening but do not know exactly what is causing it. They do believe that there is more of an environmental influence like stressful life events and chronic illness that cause depression. What happens to you as you go through life can disrupt these circuits.
Why should you care about this?
Knowing this information affects how depression will be treated in the future. According to the National Institute of Mental Health, a third of people do not respond to multiple medications, which has made treatment-resistant depression a big problem.
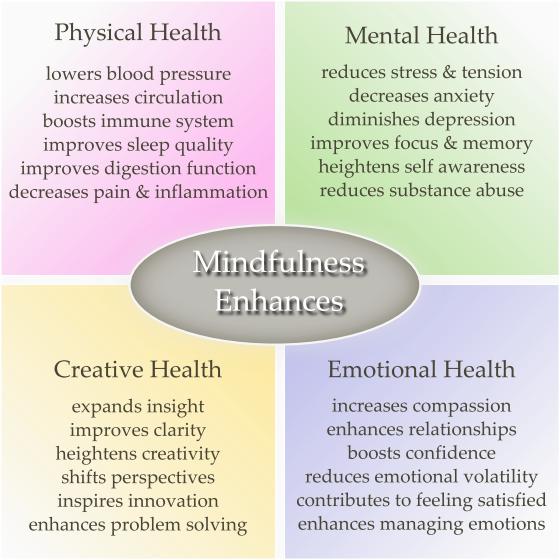
New medications are now being designed to address preventing the disruption of circuits, addressing the problem instead of the consequence. Low serotonin is the consequence, not the cause. Through all of this, researchers have gained a better understanding of how the psychotherapies of mindfulness enhance neuroplasticity and improve the connections in the circuits.
What is mindfulness?
Simply put, mindfulness is attention to the here and now. It is being fully present in the moment, and you are experiencing the present moment in a non-judgmental way. Experiencing any given moment is different from thinking about it. We spend more time thinking and processing thoughts than we do experiencing, and your mind is always working and processing a lot of thoughts every day. Thoughts can be your friend if they are creative and help you figure out problems. But thoughts can be your enemy when they make you worry, ruminate over things – which is thinking of something over and over again, and they can be your enemy when they tell you negative things about yourself. So, managing your thoughts is one of the goals of mindfulness.
Why does this matter?
In an article from Science Magazine, researchers talked about how the normal default mode your brain is to wander and think about things from the past and present. It is called stimulus-independent thought, and although this is the default mode of your brain, it comes at an emotional cost. Researchers found that people were more unhappy when their thoughts wandered than when they were intentionally thinking about the thing that was currently happening. So, an overactive mind creates dis-ease and distress. Likewise, a mind with more controlled thoughts on the present is less uneasy.
How is this related to brain function?
Researchers have shown that depression can be characterized as less connectivity between the neurons in certain parts of the brain that regulate and process your emotions. More specifically, the frontoparietal network. They also found hyper-connectivity in the default mode network in your brain.
The default mode network is a region of your brain that is responsible for self-reflection and emotional appraisal. Emotional appraisal is where you form judgments about a particular situation. For example, suppose you lose your job, and you cannot find another one. You could be sitting around thinking about your situation and start focusing on all the negative things that have happened to you, and come to the conclusion my life sucks, what’s the point? That is one appraisal. Another situation could be you are thinking about your situation and think, I hate this. I’ve got to find something else to do. Maybe I need to switch careers. What else can I do? How can I make that happen? Do I need to get more training? The first appraisal is more negative and hopeless, the second appraisal is more hopeful and problem-solving-focused.
With depression, you selectively focus on negative things and wallow in negative self-appraisal. This is rumination. You can just get lost in negative thinking. We see this with the hopelessness of depression. You get this tunnel vision that blocks out the positive thoughts, and you get locked into this negative world in your head.
So, depression equals loose connections in the frontoparietal network and tight connections in the default network. The end result is poor ability to regulate your mood and too much time ruminating on negative things.
Here’s where mindfulness comes to the rescue.
Because mindfulness helps reduce self-critical thoughts, it strengthens the connectivity in the frontoparietal network and weakens the connectivity in the default network. This, of course, is a simplified explanation. Here is a bigger point of how it can treat depression in the long run. Researchers have shown that not only does the practice of mindfulness help during the period that you are doing it, but if you practice it on a regular basis, you get sustained connectivity and, therefore, improvement in your depression.
What’s a regular basis?
In the studies, the participants completed an eight-week program of doing mindfulness exercises on average 30 minutes to an hour a day. Now I realize even 30 minutes a day is a lot, and you don’t have to start with that. But keep in mind practicing mindfulness doesn’t always have to involve sitting in a room with your eyes closed in quiet meditation. You can be in a mindful state in your day-to-day activities.
The mindfulness attention awareness scale is a questionnaire that researchers use to get a sense of a person’s baseline level of mindfulness in their everyday activities. Some of the items used to measure are as follows:
Can you relate to any of these?
These are a few examples of how you can mindlessly engage in everyday activities. The practice of mindfulness will involve not only having quiet time but learning how to be more present and aware throughout your day.
So back to the issue of whether or not it’s better than medication. For some people, it may be a better option, given the potential side effects of medication. However, it does not have to be either-or. You can practice mindfulness alongside your medication treatment. Then once your episode resolves, your mindfulness practice is something you can use to help keep you out of depression. You can see a therapist who specializes in mindfulness-based cognitive therapy. But to do this on your own, the easiest way to start is to guided meditations where you listen to someone talk you through the process.
Challenge yourself to set aside 5 to 10 minutes each day to pull away from the busyness of life and be mindful. There is a lot more to mindfulness, but for now, I hope this can help you get started.
References:
Brown, K. W., West, A. M., Loverich, T. M., & Biegel, G. M. (2011). Assessing adolescent mindfulness: validation of an adapted Mindful Attention Awareness Scale in adolescent normative and psychiatric populations. Psychological assessment, 23(4), 1023–1033. https://doi.org/10.1037/a0021338
Brunoni, A. R., Lopes, M., & Fregni, F. (2008). A systematic review and meta-analysis of clinical studies on major depression and BDNF levels: implications for the role of neuroplasticity in depression. The international journal of neuropsychopharmacology, 11(8), 1169–1180. https://doi.org/10.1017/S1461145708009309
Duman, C. H., & Duman, R. S. (2015). Spine synapse remodeling in the pathophysiology and treatment of depression. Neuroscience letters, 601, 20–29. https://doi.org/10.1016/j.neulet.2015.01.022
Farb, N. A., Anderson, A. K., & Segal, Z. V. (2012). The mindful brain and emotion regulation in mood disorders. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 57(2), 70–77. https://doi.org/10.1177/070674371205700203
Gusnard DA, Akbudak E, Shulman GL, Raichle ME. Medial prefrontal cortex and self-referential mental activity: relation to a default mode of brain function. Proc Natl Acad Sci U S A. 2001;98(7):4259-64. https://doi.org/10.1073/pnas.071043098
Kaiser, R. H., Andrews-Hanna, J. R., Wager, T. D., & Pizzagalli, D. A. (2015). Large-Scale Network Dysfunction in Major Depressive Disorder: A Meta-analysis of Resting-State Functional Connectivity. JAMA psychiatry, 72(6), 603–611. https://doi.org/10.1001/jamapsychiatry.2015.0071
Kang, H. J., Voleti, B., Hajszan, T., Rajkowska, G., Stockmeier, C. A., Licznerski, P., Lepack, A., Majik, M. S., Jeong, L. S., Banasr, M., Son, H., & Duman, R. S. (2012). Decreased expression of synapse-related genes and loss of synapses in major depressive disorder. Nature medicine, 18(9), 1413–1417. https://doi.org/10.1038/nm.2886
Killingsworth, M. & Gilbert, D. (2010). A Wandering Mind Is an Unhappy Mind. SCIENCE12 NOV 2010 : 932 https://science.sciencemag.org/content/330/6006/932.abstract
Ma, S. H., & Teasdale, J. D. (2004). Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. Journal of consulting and clinical psychology, 72(1), 31–40. https://doi.org/10.1037/0022-006X.72.1.31
Rush, A. J., Trivedi, M. H., Wisniewski, S. R., Nierenberg, A. A., Stewart, J. W., Warden, D., Niederehe, G., Thase, M. E., Lavori, P. W., Lebowitz, B. D., McGrath, P. J., Rosenbaum, J. F., Sackeim, H. A., Kupfer, D. J., Luther, J., & Fava, M. (2006). Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. The American journal of psychiatry, 163(11), 1905–1917. https://doi.org/10.1176/ajp.2006.163.11.1905
Serafini G. (2012). Neuroplasticity and major depression, the role of modern antidepressant drugs. World journal of psychiatry, 2(3), 49–57. https://doi.org/10.5498/wjp.v2.i3.49
Taylor, V. A., Daneault, V., Grant, J., Scavone, G., Breton, E., Roffe-Vidal, S., Courtemanche, J., Lavarenne, A. S., Marrelec, G., Benali, H., & Beauregard, M. (2013). Impact of meditation training on the default mode network during a restful state. Social cognitive and affective neuroscience, 8(1), 4–14. https://doi.org/10.1093/scan/nsr087
Yang, C. C., Barrós-Loscertales, A., Pinazo, D., Ventura-Campos, N., Borchardt, V., Bustamante, J. C., Rodríguez-Pujadas, A., Fuentes-Claramonte, P., Balaguer, R., Ávila, C., & Walter, M. (2016). State and training effects of mindfulness meditation on brain networks reflect neuronal mechanisms of Its antidepressant effect. Neural plasticity, 9504642. https://doi.org/10.1155/2016/9504642