This website requires you to be 21 years or older to enter. Please confirm your age below to continue.
A propaganda film from 1936 that has become a cult hit because of its dated outlook on cannabis use, Reefer Madness, is the height of camp entertainment. Framed as a “documentary,” the film’s slapstick scenes are narrated by a fictional high school principal alerting his students about what’s plaguing the nation’s youth. “Not alcoholism, not opium, not cocaine,” he declares, “but marijuana is the worst drug corrupting the youth of America.” The bulk of the film focuses on high school kids smoking pot and quickly going insane, playing “evil” jazz music, being committed, and going on a murder spree. Meant to be an important and tragic cautionary tale, this dated black-and-white film’s true value is in its many entertaining moments of unintended hilarity.
“Marijuana is the most violence-causing drug in the history of mankind” – Harry J. Anslinger
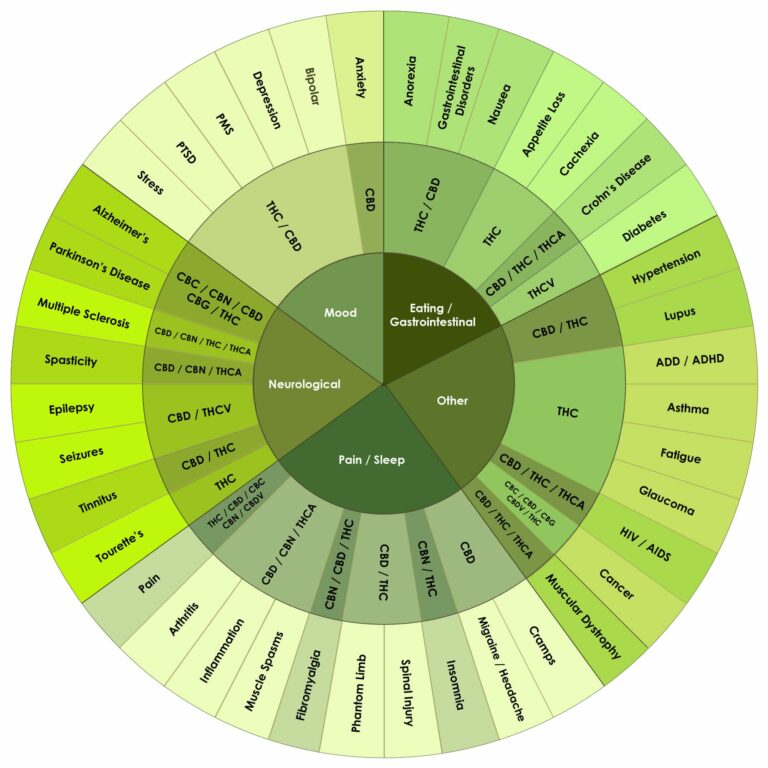
Thanks to research, we know now how ridiculous these claims are. Research from all around the world have proven and continue to demonstrate that cannabis, when taken correctly, is beneficial in helping to treat many conditions including appetite loss, nausea, cancer, neurological pain, mood disorders, and so much more.
CANNABIS THROUGHOUT TIME
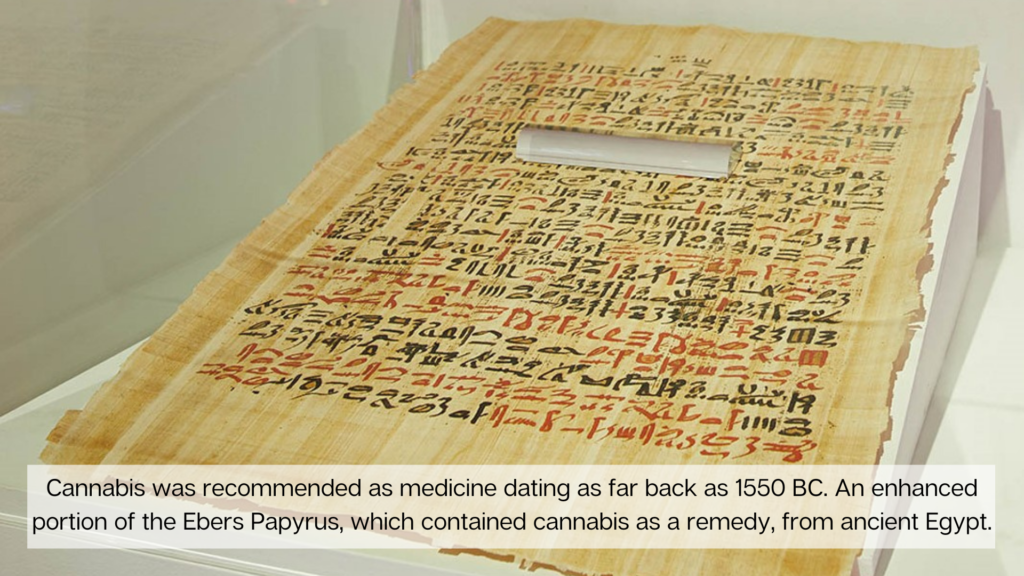
To understand how we went from madness to medicine we need to travel back to the Neolithic area (10,000 – 3,000 BC) in East Asia where Emperor Fu Hsi makes a reference to Ma, the Chinese word for cannabis, stating it was a “very popular medicine that possessed both yin and yang.”
Continuing through time, in 2700 BC, Emperor Shen Nung documents the healing properties of cannabis in China. In 1500 BC, cannabis was added to the Chinese Pharmacopeia, recommending cannabis for more than one hundred ailments, including gout, rheumatism, malaria, and absentmindedness.
Around 1450 BC, as described by the original Hebrew version of Exodus (30:22-23), references Holy anointing oil made with kaneh bosem, identified by respected etymologists, linguists, anthropologists, botanists, and other researchers as cannabis. The Egyptians used cannabis for Glaucoma and inflammation in 1213 BC.
A drink of cannabis and milk was used in India around 1000 BC to treat a wide variety of ailments including, pain, and in 600 BC, cannabis is used in India to cure Leprosy. Practitioners of traditional Ayurvedic medicine still prescribe cannabis to promote sleep, appetite, and digestion as well as to relieve pain; it is also considered an aphrodisiac and intoxicant.
By the year 1600, there are documented accounts of cannabis healing or being used to treat conditions by the Greeks, Romans, Arabic, African, and others. It is even reported that in Victorian times Queen Victoria used cannabis for menstrual cramps.
FROM MADNESS TO MEDICINE
Our historical timeline is filled with anecdotal reports of cannabis used as medicine. So, what brought the healing of cannabis to a screeching halt? Politics and greed brought on the Reefer Madness era that shut down cannabis as medicine around the world.
Since this tragic loss, scientists have been conducting research to demonstrate what the world had already known, cannabis heals.
Today thanks to research, we know that cannabis has hundreds of compounds called cannabinoids and terpenes that work synergistically with the body’s endocannabinoid system (ECS) to help provide homeostasis or balance within.
CANNABINOID SCIENCE
Cannabinoids exert their effects by interacting with specific receptors – cannabinoid receptors 1 and 2 or CB1 and CB2. These receptors are found throughout the body. CB1 receptors are mostly found in the central nervous system with an abundance in the brain. In fact, the brain has ten times more cannabinoid receptors than other pain receptors, such as morphine receptors. CB2 receptors are mostly found in the peripheral nervous system, especially immune cells.
Cannabinoids can bind to either receptor. The effects that result depend on where the receptor is located and which cannabinoid binds to it. Tetrahydrocannabinol (THC) is one of the main cannabinoids and is the one known for its euphoric effects. Once in your body, THC interacts with your ECS through binding of CB1 and CB2 receptors to reduce acute pain.
The ECS is a complex system that experts have not yet determined exactly how it works or its full function. What they do know is the ECS is linked to the following processes:
• appetite and digestion
• metabolism
• chronic pain
• inflammation and other immune system responses
• mood
• learning and memory
• motor control
• sleep
• cardiovascular system function
• muscle formation
• bone remodeling and growth
• liver function
• reproductive system function
• stress
• skin and nerve function
Today, experts believe that maintaining homeostasis (internal balance) is the primary role of the ECS. For example, if an outside force, such as pain from an injury or a fever, throws off your body’s homeostasis, your ECS kicks in to help your body return to its optimal functioning.
THE CONSEQUENCES OF REEFER MADNESS
As mentioned above, the 1930’s propaganda film, Reefer Madness, captured the essence of the anti-cannabis campaign started by Harry Anslinger, a government employee eager to make a name for himself. Now 90 years and hundreds of billions of dollars later, we are still fighting to change cannabis from an illegal drug back to the medicine we know it to be.
Cannabis could be a life-changing miracle for some patients. Unfortunately, cannabis is still classified as a Schedule I drug under the Control Substances Act, which classifies cannabis with drugs like heroin, LSD, and ecstasy. The first step is to change the schedule of cannabis.
The existing cannabis schedule presents a number of obstacles, including legal and supply concerns. We can’t fully investigate the effects or potential advantages of medical cannabis as long as it’s classified as a Schedule I substance because the medication is subject to considerable federal restrictions as a result of its classification. It is not regarded as a medicine that would provide any genuine medical advantages under the existing system. Scientists who want to perform clinical research must also jump through several hoops before beginning their study, including submitting an application to the FDA and receiving approval from the DEA. Furthermore, all research efforts must go through the National Institute on Drug Abuse, and the cannabis used must be sourced from their authorized facility.
Scientists and the public have been battling the federal government, requesting they get out of the way of research and enable the American people access to the information they need to relieve pain and perhaps save lives, particularly as the opioid crisis continues to ravage our communities.
MOVING FORWARD
To date, 18 states have legalized the recreational use of cannabis and 37 states, along with the District of Columbia, Puerto Rico, Guam, and the U.S. Virgin Islands, now allow the medical use of the cannabis plant.
In May 2021, the Drug Enforcement Administration took an important step to increase opportunities for medical and scientific research. The DEA will be allowing additional authorized entities to produce cannabis for research purposes. Currently, the National Center for the Development of Natural Products at the University of Mississippi is the only approved supplier of cannabis for research purposes in the United States, and that production has been exclusively for the National Institute on Drug Abuse.
WHERE WOULD WE BE TODAY?
Had cannabis been available, maybe we would not have the opioid crisis we have today or the fatalities that come along with it. Instead of your physician writing a prescription for an addictive and possible dangerous narcotic for pain (with side effects), you could be prescribed a few cannabinoids like CBD and THC – which are not addictive and have other positive benefits besides pain relief. Had anti-cannabis propaganda not come about, if the last 90 years and the hundreds of billions of dollars were given to researchers to study cannabis, think of where we would be today.
References
Deitch, R. (2003). Hemp: American history revised: The plant with a divided history. New York: Algora Pub, 2003. November 4, 2021. https://www.algora.com/68/book/details.html
Institute of Medicine. (2001). Marijuana As Medicine?: The Science Beyond the Controversy. Washington, DC: The National Academies Press. https://doi.org/10.17226/9586
Kogan, N. M., & Mechoulam, R. (2007). Cannabinoids in health and disease. Dialogues in clinical neuroscience, 9(4), 413–430. https://doi.org/10.31887/DCNS.2007.9.4/nkogan
National Academies of Sciences, Engineering, and Medicine. (2017). The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington, DC: The National Academies Press. https://doi.org/10.17226/24625
Pertwee R. G. (1997). Pharmacology of cannabinoid CB1 and CB2 receptors. Pharmacology & therapeutics, 74(2), 129–180. https://doi.org/10.1016/s0163-7258(97)82001-3 .
Ren, G., Zhang, X., Li, Y., Ridout, K., Serrano-Serrano, M. L., Yang, Y., Liu, A., Ravikanth, G., Nawaz, M. A., Mumtaz, A. S., Salamin, N., & Fumagalli, L. (2021). Large-scale whole-genome resequencing unravels the domestication history of Cannabis sativa. Science advances, 7(29), eabg2286. https://doi.org/10.1126/sciadv.abg2286
Richards, L. O. (1990). The Revell Bible Dictionary. Old Tappan, New Jersey: Fleming H. Revell Co. November 4, 2021
Russo, E. B., & Marcu, J. (2017). Cannabis Pharmacology: The Usual Suspects and a Few Promising Leads. Advances in pharmacology (San Diego, Calif.), 80, 67–134. https://doi.org/10.1016/bs.apha.2017.03.004
Russo E. B. (2011). Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects. British journal of pharmacology, 163(7), 1344–1364. https://doi.org/10.1111/j.1476-5381.2011.01238.x