This website requires you to be 21 years or older to enter. Please confirm your age below to continue.
Cannabinoid hyperemesis syndrome (CHS) is a rare condition caused by the long-term use of cannabis. CHS was brought to light in 2004 when a group of Australian researchers wrote about 19 chronic cannabis users who had repeated episodes of abdominal pain and retching. Ironically, many people use cannabis products to treat nausea and vomiting, so why would cannabis cause this condition?
What causes CHS?
Cannabis is a complex substance that affects everyone differently. The main ingredient in cannabis is THC, which has anti-nausea effects, and therefore cannabis is regularly prescribed for nausea caused by chemotherapy treatment. However, if used over a long period of time, cannabis seems to have the opposite effect on the digestive system and makes some consumers more likely to feel and be sick.
Unfortunately, CHS is poorly understood, and researchers are trying to understand why some people develop it while others don’t. Regular long-term cannabis use is the only known cause of CHS. The thought behind this – CHS may be a result of chronic overstimulation of endocannabinoid receptors, causing disorder in the body’s intrinsic control of nausea and vomiting.
Cannabis has several compounds which bind to different receptors throughout the body and affect the way they work or transmit information. For example, they affect the receptors found in the brain and cause the ‘high’ that users feel. They also affect the way the molecules in the gut function and can change the time it takes the stomach to empty. Cannabis also affects the esophageal sphincter, which is the tight band of muscle that opens and closes to let food pass from the esophagus (food pipe) into the stomach. The effects of cannabis on your digestive system are what lead to the main symptoms of CHS.
Another thought is that genetics may play a role because only a small number of people who regularly use cannabis develop CHS.
What are the symptoms?
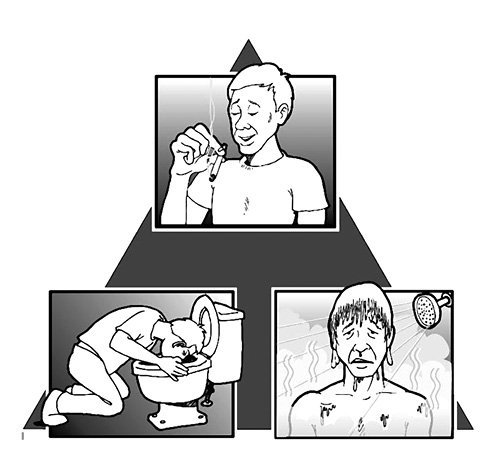
There are three phases of CHS, the prodromal phase, hyperemetic phase, and recovery phase.
The prodromal phase can last for weeks, months, or years. Symptoms include abdominal discomfort, fear of vomiting, early morning nausea without vomiting. Other symptoms that vary in severity include anxiety, sweating, flushing, and increased thirst. These symptoms tend to be more severe in the morning.
The hyperemetic phase is characterized by reoccurring and often overwhelming nausea, vomiting, and debilitating abdominal pain. Other symptoms in this stage are dry heaving, decreased food intake, anxiety, dehydration, and compulsive bathing or showering in hot water to ease symptoms. This phase will last until prolonged abstinence from cannabis has occurred and CHS patients enter a recovery phase where vomiting and bathing behavior subsides.
The recovery phase will begin once you stop using cannabis. During this phase, the symptoms will go away, and you will be able to eat normally again. This phase can be unique to the individual and last for days or months. Most consumers found if they started to use cannabis again, the symptoms returned.
How is CHS diagnosed?
CHS is a diagnosis based on ruling out other hyperemetic conditions such as hyperemesis gravidarum, psychogenic vomiting, or cyclic vomiting syndrome.
In 2012 researchers presented the diagnostic criteria, based on symptoms and patient behavior, as part of a large case study. The prerequisite for a CHS diagnosis is long-term use of cannabis, abdominal pain, severe and reoccurring episodes of nausea and vomiting that is relieved with hot showering or completely abstaining from cannabis.
How is cannabis hyperemesis syndrome treated?
Currently there are no standard treatments. Abstaining from cannabis use is the only way to stop CHS. Your doctor may recommend several other treatments to alleviate your symptoms along with quitting cannabis. Anxiolytics (anxiety medication), sedatives, and antipsychotics seem to be the most effective – but it is unclear whether these medications are effective because they interfere with the mechanism of CHS or because their sedating effects.
Conclusion
Excessive cannabinoid administration disrupts the normal functioning of the endocannabinoid system, which may cause CHS. More clinical and pre-clinical research is needed to fully understand the underlying pathophysiology of this disorder and the negative consequences of prolonged high-dose cannabis use.
References
Allen, J. H., de Moore, G. M., Heddle, R., & Twartz, J. C. (2004). Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis abuse. Gut, 53(11), 1566–1570. https://doi.org/10.1136/gut.2003.036350
DeVuono MV, Parker LA (2020) Cannabinoid hyperemesis syndrome: a review of potential mechanisms, Cannabis and Cannabinoid Research 5:2, 132–144, DOI: http://doi.org/10.1089/can.2019.0059
Figueroa-Rivera, I. M., Estremera-Marcial, R., Sierra-Mercado, M., Gutiérrez-Núñez, J., & Toro, D. H. (2015). Cannabinoid Hyperemesis Syndrome: A Paradoxical Cannabis Effect. Case reports in gastrointestinal medicine, 2015, 405238. https://doi.org/10.1155/2015/405238
Galli, J. A., Sawaya, R. A., & Friedenberg, F. K. (2011). Cannabinoid hyperemesis syndrome. Current drug abuse reviews, 4(4), 241–249. https://doi.org/10.2174/1874473711104040241
Kelly, J. F., Yeterian, J. D., Cristello, J. V., Kaminer, Y., Kahler, C. W., & Timko, C. (2016). Developing and Testing Twelve-Step Facilitation for Adolescents with Substance Use Disorder: Manual Development and Preliminary Outcomes. Substance abuse : research and treatment, 10, 55–64. https://doi.org/10.4137/SART.S39635
Lapoint, J., Meyer, S., Yu, C. K., Koenig, K. L., Lev, R., Thihalolipavan, S., Staats, K., & Kahn, C. A. (2018). Cannabinoid Hyperemesis Syndrome: Public Health Implications and a Novel Model Treatment Guideline. The western journal of emergency medicine, 19(2), 380–386. https://doi.org/10.5811/westjem.2017.11.36368
Moon, A. M., Buckley, S. A., & Mark, N. M. (2018). Successful Treatment of Cannabinoid Hyperemesis Syndrome with Topical Capsaicin. ACG case reports journal, 5, e3. https://doi.org/10.14309/crj.2018.3
Richards, J. R., Gordon, B. K., Danielson, A. R., & Moulin, A. K. (2017). Pharmacologic Treatment of Cannabinoid Hyperemesis Syndrome: A Systematic Review. Pharmacotherapy, 37(6), 725–734. https://doi.org/10.1002/phar.1931
Simonetto, D. A., Oxentenko, A. S., Herman, M. L., & Szostek, J. H. (2012). Cannabinoid hyperemesis: a case series of 98 patients. Mayo Clinic proceedings, 87(2), 114–119. https://doi.org/10.1016/j.mayocp.2011.10.005
Sun, S., & Zimmermann, A. E. (2013). Cannabinoid hyperemesis syndrome. Hospital pharmacy, 48(8), 650–655. https://doi.org/10.1310/hpj4808-650
Venkatesan, T., Levinthal, D. J., Li, B., Tarbell, S. E., Adams, K. A., Issenman, R. M., Sarosiek, I., Jaradeh, S. S., Sharaf, R. N., Sultan, S., Stave, C. D., Monte, A. A., & Hasler, W. L. (2019). Role of chronic cannabis use: Cyclic vomiting syndrome vs cannabinoid hyperemesis syndrome. Neurogastroenterology and motility : the official journal of the European Gastrointestinal Motility Society, 31 Suppl 2(Suppl 2), e13606. https://doi.org/10.1111/nmo.13606